Frozen shoulder
Frozen shoulder (adhesive capsulitis) is stiffness, pain, and limited range of movement in your shoulder. It may happen after an injury or overuse or from a disease such as diabetes or a stroke. The tissues around the joint stiffen, scar tissue forms, and shoulder movements become difficult and painful. The condition usually comes on slowly, then goes away slowly over the course of a year or more.
Causes of frozen shoulder
The cause of frozen shoulder is not fully understood and in some cases is unidentifiable. However, most people with frozen shoulder have suffered from immobility as a result of a recent injury or fracture. The condition is common in people with diabetes.
Risk factors for frozen shoulder
A risk factor is something that elevates the risk of developing a disease or condition. For example, smoking is a risk factor for cancer – it elevates the risk of developing lung cancer.
Common risk factors for frozen shoulder are:
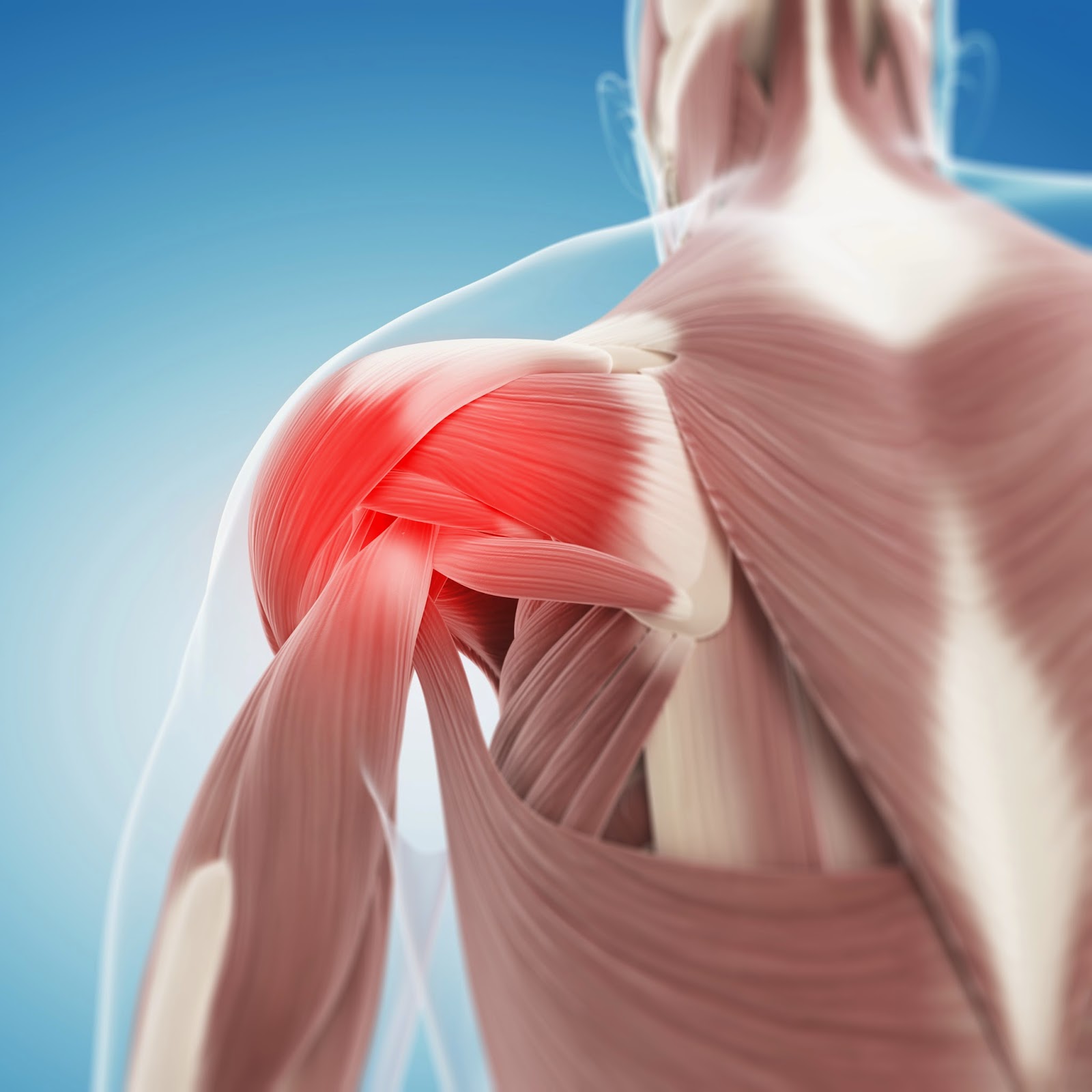
A woman suffering with shoulder pain
You’re more likely to suffer from frozen shoulder if you’re female and over 40 years of age.
Age – being over 40 years of age.
Gender – 70% of people with frozen shoulder are women.
Recent surgery or arm fracture – immobility of recovery may cause the shoulder capsule to stiffen.
Diabetes – two to four times more likely to develop frozen shoulder for unknown reasons; symptoms may be more severe.
Having suffered a stroke.
Hyperthyroidism (overactive thyroid).
Hypothyroidism (underactive thyroid).
Cardiovascular disease (heart disease).
Parkinson’s disease.
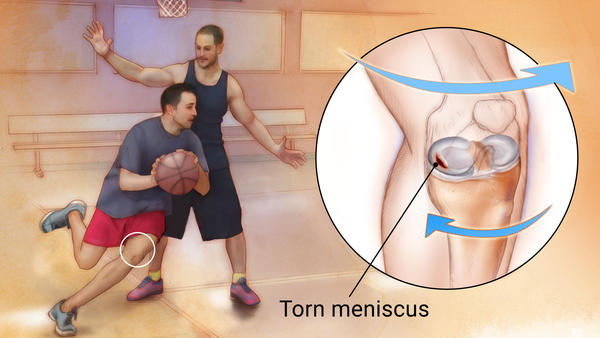
Symptoms of frozen shoulder
A symptom is something the patient feels and/or reports, while a sign is something others, including the doctor observe. For example, pain is usually a symptom, while a rash could be a sign.
The most pervasive sign or symptom of frozen shoulder is a persistently painful and stiff shoulder joint. Signs and symptoms of frozen shoulder develop gradually; usually in three stages in which signs and symptoms worsen gradually and resolve within a two – year period.
There are three stages of frozen shoulder:
Painful stage – the shoulder becomes stiff and then very painful with movement. Movement becomes limited. Pain typically worsens at night.
Frozen/adhesive stage – the shoulder becomes increasingly stiff, severely limiting range of motion. Pain may not diminish, but it does not usually worsen.
Thawing stage – movement in the shoulder begins to improve. Pain may fade, but occasionally recur.
Diagnosis of frozen shoulder
Doctors will most likely diagnose frozen shoulder based on signs and symptoms and a physical exam; paying close attention to the arms and shoulders. The severity of frozen shoulder is determined by a basic test in which a doctor presses and moves certain parts of the arm and shoulder.
Structural problems can only be identified with the help of imaging tests, such as an X – ray or MRI. An X-ray is a type of electromagnetic radiation that can penetrate most solid objects to create images of an object’s interior. An MRI (magnetic resonance imaging) uses magnetic signals to create image “slices” of the soft tissues inside the human body.
Treatment options for frozen shoulder
The aim of treatment for frozen shoulder is to alleviate pain and preserve mobility and flexibility in the shoulder.Recovery may be slow, as symptoms tend to persist for several years.
Treatment options for frozen shoulder include:
Painkillers – relieve symptoms of pain. Nonsteroidal anti – inflammatory drugs (NSAIDs), such as ibuprofen, are over the counter (OTC, no prescription required) painkillers and may reduce inflammation of the shoulder in addition to alleviating mild pain. Acetaminophen (paracetamol, Tylenol) is recommended for extended use. Prescription painkillers, such as codeine (an opiate – based painkiller) may also reduce pain. Not all painkillers are suitable for every patient; be sure to review options with your doctor.
Exercise – frequent, gentle exercise can prevent and even reverse stiffness in the shoulder.
An ice pack applied to a man’s shoulder
Alternating between hot and cold compression packs can help with frozen shoulder
Hot or cold compression packs – help to reduce pain and swelling. It is often helpful to alternate between the two.
Corticosteroid injections – a type of steroid hormone that reduces pain and swelling. Corticosteroids may be injected into the shoulder joint to alleviate pain, especially in the ‘painful stage’ of symptoms. However, repeated corticosteroid injections are discouraged as they could cause damage to the shoulder.
Transcutaneous electrical nerve stimulation (TENS) – numbs the nerve endings in the spinal cord that control pain and sends small pulses of electricity from the TENS machine to electrodes (small electric pads) that are applied to the skin on the affected shoulder.
Physical therapy – can teach you exercises to maintain as much mobility and flexibility as possible without straining the shoulder or causing too much pain.
Shoulder manipulation – the shoulder joint is gently moved while you are under a general anesthetic (a drug that makes you completely unconscious).
Shoulder arthroscopy – a minimally invasive type of surgery used in a small percentage of cases. A small endoscope (tube) is inserted through a small incision into the shoulder joint to remove any scar tissue or adhesi